No Surprises Act Arbitration and Recovery Services
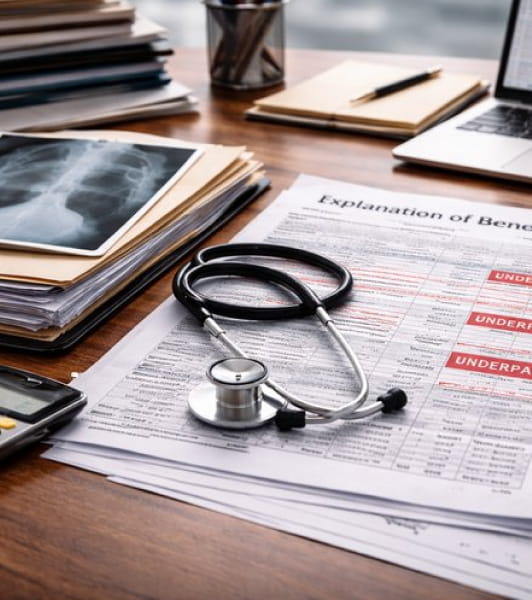
The No Surprises Act created one of the most important financial protection systems for out-of-network providers in modern healthcare.
When insurers issue low initial payments, deny legitimate emergency cases, or reduce complex procedures without support, you now have a federal pathway to challenge those reductions and recover revenue you previously wrote off. This is why providers across the country rely on No Surprises Act expert representation to navigate federal Independent Dispute Resolution (IDR) and secure full payment for their work.
If you need to appeal underpaid NSA reimbursement or contest an NSA initial insurer payment, you strengthen your outcome with a structured approach. You can use federal arbitration to escalate disputes, present the medical evidence, and secure a final, binding determination. Many organizations request help when they need to file an NSA arbitration claim, prepare an NSA arbitration submission, or draft an NSA claim evidence package, especially when the case involves emergency care or complex procedures. You also gain support through healthcare revenue recovery under the No Surprises Act, which allows you to recover substantial amounts across multiple high-value claims.
This page explains what the No Surprises Act process involves, why it matters for your revenue, who benefits most from this support, and what you gain when you choose a specialized NSA claims review and recovery partner like Callagy Recovery.
What Is the No Surprises Act?
The No Surprises Act is a federal law designed to protect patients from unexpected out-of-network bills and to protect providers from unfair insurer underpayments. When you deliver emergency care or treat patients at in-network facilities, insurers must issue a reasonable initial payment. When that payment falls short of the appropriate value, you escalate the dispute through Independent Dispute Resolution.
NSA arbitration is a legally binding federal process that allows you to present evidence showing the true value of your services. You use that process when you need NSA arbitration representation services or provider representation in NSA disputes, especially when they require advanced documentation and strategic positioning. You may also use NSA arbitration when you need independent dispute resolution help with Federal NSA expertise, particularly in situations where emergency care is involved.
The process begins when you initiate an insurance underpayment appeal under the No Surprises Act. A certified federal arbitrator reviews your case by examining medical complexity, coding accuracy, benchmark comparisons, and all supporting documentation. You strengthen your position by submitting a complete file that shows the full clinical narrative, financial justification, and coding integrity behind each claim.
The No Surprises Act is a federal protection for you, and it gives you a pathway to recover revenue at scale.
Why the No Surprises Act Matters for Providers
The No Surprises Act significantly shifts the balance of power in reimbursement disputes. Insurers can no longer reduce emergency and facility-based out-of-network claims without scrutiny. You now have the chance to submit an NSA claim dispute for underpaid claims. This process requires them to justify their payment amounts and prove they followed federal rules.
You gain several advantages:
- You receive a final, binding decision from a neutral arbitrator.
- You secure outcomes that are enforceable at the federal level.
- You improve consistency in high-acuity emergency claim recovery.
- You strengthen financial performance across your out-of-network portfolio.
- You build long-term leverage when payers know that your cases escalate successfully.
You rely on NSA support when you need to resolve denied NSA claims, recover funds via the NSA process, or pursue denied claim recovery under the No Surprises Act for emergency patients treated without the ability to check network status.
You also improve your revenue cycle when you pursue medical claim underpayment recovery under the No Surprises Act, which helps you correct reduced payments across high-value cases. This system protects the work your team performs and confirms insurers recognize the full clinical and financial reality of your services.
Who We Represent Under the No Surprises Act
Hospitals
Hospitals experience significant underpayments in trauma cases, emergency interventions, surgical procedures, imaging bundles, and facility-based care. You gain strong outcomes when you pursue hospital claim recovery services with Federal NSA expertise to correct initial payments and secure the full value of your encounters.
Medical Groups
Emergency physicians, anesthesiologists, radiologists, and specialty groups frequently use NSA arbitration to correct steep reimbursement reductions. You benefit from leveraging NSA recovery services and NSA recovery advocates for providers that improve outcomes for groups facing consistent payer cuts.
Surgeons & Trauma Providers
Surgeons frequently need to challenge reduced out-of-network payments, downcoded procedures, and improper bundling. You receive leverage through OON claim recovery under the No Surprises Act and, when applicable, OON claim recovery under the No Surprises Act with no upfront cost depending on contingency engagement terms.
Surgical Centers
Surgical centers experience reductions in both facility and professional components. You strengthen your case when you pursue out-of-network claim recovery under the No Surprises Act.
Emergency Care Providers
Emergency providers rely on NSA protections frequently. When the initial payment does not reflect the medical intensity of your services, you benefit from emergency care reimbursement under the No Surprises Act, supported by arbitration specialists who understand emergency documentation.
How Federal NSA Arbitration Works
Federal NSA arbitration follows a strict timeline and includes the following steps:
Initial Payment Review
You verify the insurer’s initial payment and determine whether it aligns with the complexity and value of your service. If not, you escalate the claim.
Open Negotiation Period
You formally request higher reimbursement. If the payer does not respond adequately, you advance the case to arbitration.
Federal IDR Filing
You escalate your dispute through the federal portal when you need to file an NSA arbitration claim, request an NSA claims evaluation, or initiate an NSA claim dispute for underpaid claims. This step requires careful documentation.
Evidence Submission
You compile a complete case file and prepare an NSA arbitration submission with clinical narratives, benchmark comparisons, and coding support.
Arbitrator Review
A certified federal arbitrator evaluates both sides and selects the most reasonable offer. This decision is binding.
You improve every step of this process when you use full-service NSA arbitration provider support. You also gain efficiency when you rely on outsourced NSA arbitration representation, which provides full administrative, clinical, and strategic support behind each case.
Arbitration Types Covered by the NSA
The No Surprises Act governs a specific set of billing scenarios where providers can dispute low insurer payments through the federal Independent Dispute Resolution process. You can access arbitration when the encounter meets federal criteria, the plan type qualifies, and the service falls into one of the categories below. Each category links to a dedicated page that explains your recovery options in detail.
Emergency Care Reimbursement
You may qualify for emergency care reimbursement under the No Surprises Act if you deliver stabilizing treatment, trauma care, or acute interventions without confirming network status.
Out-of-Network Claim Recovery
When you treat patients at an in-network facility but remain out-of-network with the insurer, your claim may qualify for out-of-network claim recovery under the No Surprises Act if the initial payment does not reflect the value of your services.
Medical Claim Underpayment Recovery
When insurers reduce payments without justification for out-of-network emergency or facility-based care, you can leverage medical claim underpayment recovery under the No Surprises Act.
Insurance Underpayment Appeals Under the No Surprises Act
Insurers must issue a reasonable initial payment. When they do not, you may escalate the claim to arbitration through the NSA pathway to correct improper reductions.
Hospital Claim Recovery Services
Hospitals use NSA arbitration to recover revenue across high-acuity emergency encounters, surgical procedures, and facility-based out-of-network claims.
Independent Dispute Resolution (Federal IDR) Services
Federal IDR is the formal arbitration mechanism of the NSA. When a claim qualifies, this is the final, binding pathway to correct underpayments from self-funded and applicable fully insured plans.
NSA Arbitration Representation Services
If you want to outsource the entire NSA dispute process—including filing, evidence preparation, document assembly, and arbitrator communication—you can rely on full-service representation.
FAQs About the No Surprises Act
What types of disputes qualify for arbitration under the No Surprises Act?
You may escalate disputes to federal arbitration when you provide emergency care, facility-based out-of-network services, or post-stabilization services that meet NSA criteria. These disputes qualify when insurers issue reduced initial payments, deny claims that meet federal protections, or apply internal pricing that does not reflect the clinical complexity of the encounter.
How do I know if my claim qualifies for federal NSA arbitration instead of state-level arbitration?
Your eligibility depends on the patient’s insurance plan type and the state where the services were rendered. ERISA self-funded plans nearly always route through federal NSA arbitration. Fully insured plans may fall under state laws if the state operates its own arbitration system. States without a qualifying program default to federal IDR when the encounter meets NSA requirements.
Can I dispute an insurer's initial payment if it seems too low?
Yes. When the initial payment does not represent the reasonable value of your services, you can contest the NSA’s initial insurer payment with a strategy that includes open negotiation and escalation to federal IDR. You strengthen your position with a well-prepared evidence package that illustrates medical complexity and coding accuracy.
How does the No Surprises Act protect providers financially?
The NSA protects you by creating a federal mechanism to challenge unfair reductions. When insurers issue incorrect payments, you gain access to No Surprises Act expert representation and arbitration procedures that require both sides to justify their offers. The arbitrator selects the more reasonable payment, which often results in a significantly improved outcome for providers.
What documentation improves NSA arbitration outcomes?
You strengthen your position with detailed clinical narratives, complete operative notes, accurate coding, benchmark comparisons, and a cohesive presentation of medical necessity. Using the support of an NSA claim representation company to draft an NSA claim evidence package helps ensure every component is organized for arbitrator review.
Are NSA arbitration services available with no upfront cost?
Some providers qualify for contingency-based structures. This applies to claims where the recovery potential is strong and documentation supports escalation. In these cases, you may use contingency-based NSA representation or OON claim recovery under the No Surprises Act with no upfront cost, depending on eligibility.
Do hospitals benefit from NSA representation?
Hospitals often benefit significantly because emergency encounters, trauma activations, imaging, surgical services, and high-acuity cases frequently fall under NSA protections. When those claims are underpaid, you gain support from hospital claim recovery services with Federal NSA expertise to secure appropriate reimbursement.
Does the NSA apply to out-of-network providers?
Yes. When you deliver emergency services or treat patients at in-network facilities, your out-of-network status does not prevent you from using the federal process. You gain access to out-of-network claim recovery under the No Surprises Act and have the ability to escalate cases when insurers issue reduced payments.
How quickly should I act on an NSA claim?
Federal NSA disputes follow strict timelines. You must initiate open negotiation promptly and escalate to arbitration within the required window. Missing a deadline prevents escalation, so many providers rely on NSA arbitration representation services to ensure timely filings and complete documentation.
How does Callagy Recovery support the NSA arbitration process?
Callagy Recovery offers complete support, from conducting NSA claims reviews and recovery to preparing NSA arbitration submissions and providing representation throughout the arbitration process. You gain strategically assembled case files, guidance through each step, and full support from a team with deep federal NSA expertise. We position your cases accurately and competitively for arbitrator review.
Why You Should Choose Callagy Recovery for NSA Arbitration and Recovery
With Callagy Recovery, you gain a partner who understands the regulatory and procedural complexities behind NSA arbitration. You work with a team that delivers highly structured NSA arbitration representation services, evidence-driven documentation support, and complete management of the federal IDR process.
You gain advantages such as:
- A federal-only specialization that aligns with NSA requirements
- Full review of insurer’s initial payment methodologies
- Detailed case file preparation backed by coding, clinical, and legal insight
- A proven approach for underpaid emergency and OON claims
- Assistance in drafting NSA claim evidence packages with all required elements
- Strategic guidance when you need to consult on NSA arbitration strategy
- Comprehensive No Surprises Act filing support
- A clear path to appeal underpaid NSA reimbursement
- Dedicated professionals delivering third-party NSA representation solution support
You receive guidance from professionals who understand the full breadth of federal NSA rules and the nuances of high-value clinical documentation. This system improves your outcomes and ensures your team receives the reimbursement it has earned.
Callagy Recovery offers industry-leading expertise in provider representation in NSA disputes, giving you the support and structure necessary to succeed in federal arbitration.
Best of all, Callagy Recovery operates on a contingency basis. We offer out-of-network claim recovery under the No Surprises Act with no upfront cost, meaning we don’t get paid until you do.
Claim Your Full Reimbursement With Callagy Recovery
Strengthen your revenue recovery and take control of your federal arbitration strategy. Book a consultation with Callagy Recovery to evaluate your NSA cases and learn how expert support can help you recover underpaid or denied out-of-network claims.